Facts & Figures: Obesity Statistics in the UK

We've written countless blog posts about obesity statistics in the UK in the past. But we've never written a blog post compiling all of our statistics together.
We decided to do just that. In this blog post you'll find 5 years worth of obesity statistics and surveys detailing the obesity crisis in the UK.
Shocking Obesity Statistics in the UK
Treating obesity is currently costing the NHS more than £6.1billion per year, and this could increase for future generations if action isn’t taken to reduce the crisis. Obesity is also expected to have a serious impact on economic development, with an overall cost of obesity to wider society estimated at £27 billion.
The NHS is projected to spend £9.7 billion per year on overweight and obese patients by 2050, with wider costs to society estimated to reach £49.9 billion per year.
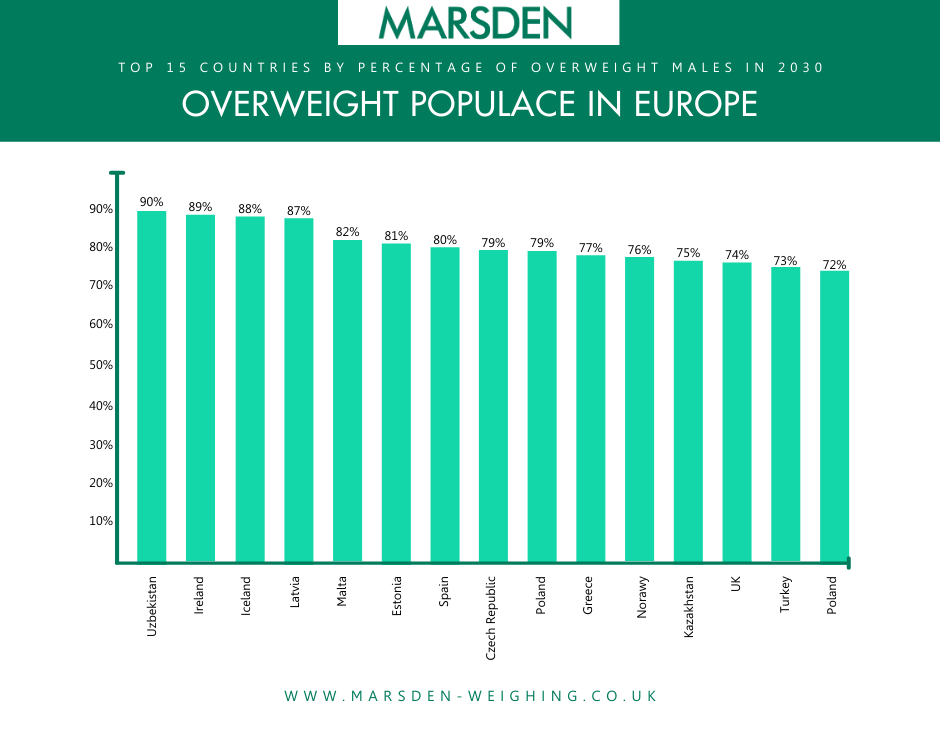
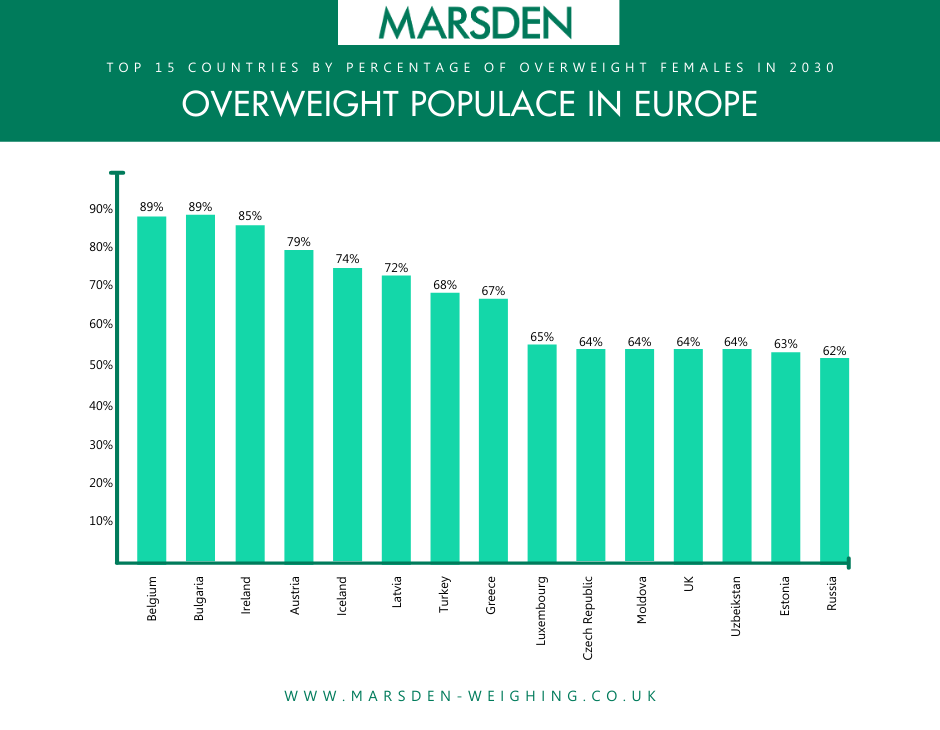
Furthermore, studies show that the UK is one of the most overweight countries in Europe, with nearly three in every four men and almost two in every three women expected to be overweight by 2030.
Furthermore it's estimated that 30% of women and 36% of men in the UK will be obese, with a BMI over 30, by 2020.
This is made worse by the fact that a poll conducted for the National Obesity Forum found only 6 per cent of Britons consider themselves obese, and almost half think they are a healthy weight. This shows that there’s not enough awareness surrounding obesity.
Childhood obesity is especially alarming, with an estimated 41 million children under 5 years old worldwide, either obese or overweight. BBC News states that more than one in 10 children in Scotland started school as obese or overweight. While this is lower in England, we still have over one in five children, who are overweight or obese before they start primary school. By the time they leave, this is one in three.
The epidemic prompted a UK politician to compare the risk posed by obesity to that of terrorism. Conservative MP, Maggie Throup, who sits on the Health Select Committee, said “brave and bold action” is required.
“I make no apologies for talking about obesity again in this chamber because, alongside terrorism and antimicrobial resistance I feel that obesity poses a major threat to our nation. Our children, our future generations, are at risk of developing serious health conditions such as Type 2 diabetes, heart disease and cancer.”
The NHS saw an 18% increase in obesity related admissions from 2016 to 2017. That’s a total of 617,000 obesity related admissions - two-thirds of which were women.
Role of Pharmacies and GPs
According to our survey, 66% of GPs and pharmacies see four or more obese patients every day - despite a third of patients understanding the health risks of being overweight.
Our survey also highlighted the main causes of obesity as processed food and lack of exercise. Patients not taking responsibility for either their own or their children’s health, TV advertising and the cost of healthy food were also cited as major factors.
The National Obesity Forum has recently outlined how pharmacists could help curb the obesity epidemic.
Risks of Being Overweight or Obese
Migraines
A study by Dr B Lee Peterlin of John Hopkins University School of Medicine found that people with obesity had a 27% higher rate of a migraine than people with a healthy weight.
Being underweight can also increase your chances of a migraine – people with a BMI less than 18.5 had a 13% higher risk than healthier
Cancer
Obesity can lead to long-term health problems, with fifteen cancers connected to it – including breast cancer, liver cancer and colon cancer.
Effects on Babies
20% of women in the world, who are of a reproductive age, are estimated to be obese. Children born to obese mothers are at a higher risk of developing heart disease, diabetes, stroke, and asthma in their lifetime.
Additionally, overweight pregnancies also increase the risk of miscarriages, blood clots and premature pregnancy.
Health experts have also described this as a ‘vicious cycle’, as overweight mothers pass obesity onto their children.
Heart Failure
Research from UT Southwestern Medical Centre has found evidence that excess weight is linked to hard-to-treat heart failures.
Being overweight - and not exercising - is strongly associated with the most severe forms of heart failure, the Medical Centre has found.
Incidents of heart failure were 19% higher for individuals who do not exercise at recommended levels - and a similar trend was found with BMI - their research stated.
Dr Jarett Berry, Associate Professor of Internal Medicine at UT Southwestern, said: “Previous studies have consistently found an association between low levels of physical activity, high BMI and overall risk of heart failure.
“But this study shows that the association is more pronounced for heart failure with ejection fraction - the type of heart failure that is most challenging to treat.”
Death
Obesity causes 47% more early deaths than tobacco – according to research by Cleveland Clinic and the New York University School of Medicine.
The researchers said that tobacco would have topped the list if it wasn’t for the global push to limit cigarette use – and experts are calling for a similar push on obesity.
What Can Be Done?
Encourage patients to attend slimming clubs
A study by University of Oxford says patients who receive advice about their weight, particularly those that are referred to slimming clubs, are more likely to actually lose weight.
The university research consulted 1882 people who had sought their GP for weight loss advice. 50% of those contacted then attended weight loss classes, the other 50% were left to diet alone.
The results showed that course attendees lost on average 1.36kg (3lb) more than those who did not attend.
Sending patients to independent slimming classes could also reduce strain on the NHS, compared to other methods of treatment – as independent consultation reduces the need to visit a GP or doctor.
It also means those required to lose weight can do so alongside others in the same position, which can help increase motivation.
Default weighing at GPs
The government believes that when GPs see a patient, weighing should take place ‘by default’. If a patient’s weight is monitored and recorded accurately, obesity rates may be reduced. Weighing should be the first and most regular way of monitoring a patient’s health, and will help to see the biggest changes in childhood obesity over the next two years.
Regular weight readings means GPs can react more easily to changes in weight and keep it within a healthy range. It also means that GPs can better judge the health of the patient, the effectiveness of medicines and enable better calculations of the remedies needed.
Talk to Patients
The report also recommends that health professionals should ‘build on the good work they already do’, by ‘always’ bringing up the family diet when talking to patients - according to GP online.
This can be difficult to do and may be uncomfortable for some, which is why the Health Education England (HEE) and Public Health England (PHE) have also launched advice for healthcare professionals when raising the issue with patients.
Raising Awareness Surrounding Obesity
In a blog post about obesity and weight loss, Pharmacy Management Magazine highlighted that obesity awareness needs to be higher - many people who are overweight are actually unaware of it.
To help pharmacies and GPs with increasing awareness of obesity, what the side effects are and how to know if you are overweight, Marsden has produced a free A3-sized obesity awareness poster.
The ‘Am I Overweight?’ poster, which you can download below, gives your customers and patients an understanding of the dangers of being overweight or obese, and a chart so they can work out if you are a healthy weight. The chart highlights the ideal BMI based on height and weight.
Download our ‘Am I Overweight?’ poster by clicking below.
Marsden Scales
Marsden offers a range of Class III Approved medical weighing scales to suit almost any patient.
The Marsden M-550 has five times the accuracy of traditional mechanical scales and features a large weighing platform. With a capacity of 160kg and graduations of 200g<100kg>500g, it can weigh most patients easily.
There's also a bluetooth version available for the easy transfer of data to a patient's record.
The Marsden M-100 Column Scale comes with either an integrated manual height measure or an integrated automatic height measure to make calculating the BMI of your patients simpler than ever before.
With a capacity of 300kg and accuracy of just 50g (increasing to 100g over 100kg), the M-100 is the perfect scale for GP surgeries and outpatient clinics.
The space-saving design means it can be stored easily in the corner of a room and not create any hazards.
The Marsden M-530 is our high capacity floor scale, with an extra wide base for use with bariatric patients.
This plus sized scale has a maximum capacity of either 300kg or 500kg, and is even more accurate than the M-550. It also has an Ultra-low profile weighing platform, to make it easy for patient to step on to and off the scale.
View more of our bariatric scales here.
Further Reading
Find out more about The ‘Obesity: An Emerging Menace’ summit and what we learned here.
We created an Obesity Awareness Poster to be used in Doctor's offices and pharmacies. Download yours here.
When working out whether you are a healthy or unhealthy weight, should you calculate BMI or body fat? Find out the positives and negatives of each in this blog post.